22 Mar, 2023
views
The Story of Resistance
by

Ashrafi Anjuman Sneha
~6 min read
Share this blog

Sitting in that hospital chair, as I waited for my uncle's verdict in his fight against death. As the bacteria in his lungs resisted with all its might, I noticed more with similar stories. It's a common theme in these hospital walls, the antibiotics aren’t effective. Patients of all ages suffer endlessly for various lengths of time in the Intensive Care Unit from these "superbugs" as their stressed family members pray, plead and negotiate with God and the next most powerful being in their eyes- the Doctor; The tireless attempts of whom fail to ease the despair in the hearts of these loved ones.
I pretended not to notice when my uncle needed blood more frequently; Septicemia, I subconsciously recalled. I told my cousin it would be alright as their visits to the ICU grew more frequent and urged. I wondered as he went through several operative procedures, about how responsible he had always been with medication. My uncle had acquired the infection right after finishing the construction of his beloved new house. He would humbly break the bricks for his own walls. Somewhere along the line a strain of multi-resistant bacteria had entered his body and began to shut it down not long after he moved into his much-awaited home, meaning he received combinations upon combinations of antibiotics which ultimately failed to be effective. It wasn't just him, I heard similar accounts of multi-resistant infections related to construction throughout the hospital.
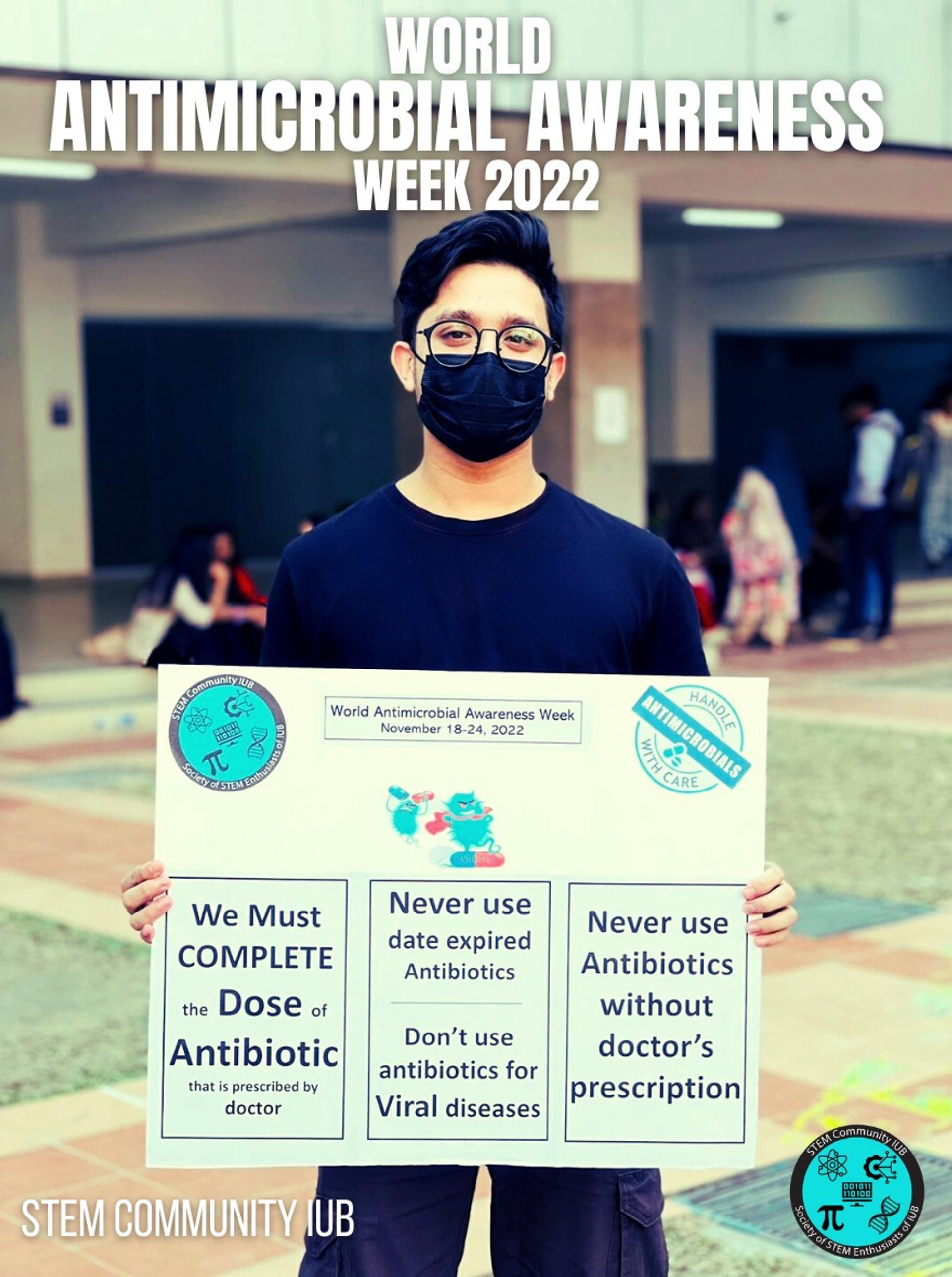
I realized it wasn't up to individuals, humans collectively contribute to the formation of drug-resistant microbes. These microorganisms rapidly adapt and grow resistant to drugs, often multiple of them, exhausting our already limited stock of antibiotics, and along with it, our hope. This isn't just constrained within our own bodies. Then, more than ever I realized, with every unprescribed antibiotic sold over the counter, every course left incomplete as soon as we feel remotely well enough, and every antibiotic disposed unsafely into the environment, we facilitate the emergence of these resistant and multi-resistant strains of microbes that eventually cripple a hundred years of medical progress.
We all know it, but we don't understand the magnitude of the situation. There are only a few new antibiotics in progress, and market forces alone cannot meet the needs of the growing list of multi-resistant microbes in need of new drugs. Priority lists of pathogens have been constructed, and placed by WHO, as an attempt to address the urgency of the matter. However, it is limited by resources, and funds.
Currently, every year, more than 700,000 people die due to drug-resistant diseases all over the world, 230,000 of whom die from multidrug-resistant strains. In Bangladesh, every year 80% of the deaths occurring in the Intensive Care Units (ICUs) are due to these supposed "superbugs". Although these resistant and multi-resistant microbes are frequently found in hospitals and care homes, South-Asian countries like Bangladesh have several drivers of antimicrobial resistance. This is due to several factors including the unnecessary and unregulated use of drugs, self-medication, incorrect prescription of medicine, poor quality of these antibiotics, lack of implementation of restrictions to the sale of antibiotics over the counter, and the use of antibiotics meant for humans as a growth factor in animals.
This eventually leads to the rapid development and accumulation of resistance as the microorganisms in our bodies and the environment increasingly come into contact with these drugs, but not enough to kill them all.
Moreover, antimicrobial drugs are very specific in the kind of microbes they combat; For instance, antibiotics do not work on viruses, hence it is not only useless against the common cold or flu, but also disrupt the body's balance of natural flora or microbiota, especially in the case of broad-spectrum antibiotics. The natural flora of our bodies is an integral part of our immune defense system and have vital roles in competing with harmful microbes, essentially preventing them from taking over. However, when this balance is destroyed, it may lead to several opportunistic diseases, weakening our immune systems and other detrimental functions like the formation of vitamin-B by our gut microbes. Narrow-spectrum antibiotics are more specifically target some particular bacteria in contrast to broad-spectrum antibiotics that destroy microbes all over a wide range of bacteria. However, they are equally effective.
Another profoundly important factor that is often overlooked in all countries, especially South-Asian countries like Bangladesh, is the correct and safe disposal of antibiotics. We often dump or flush away open antimicrobial drugs and it comes into direct contact with soil or water, and hence the microorganisms residing in them. This greatly accelerates the emergence of resistant strains through rapid mutations and transfer of genes with microorganisms like bacteria, resulting in increased morbidity and mortality as well as an increased economic burden to the health care system. Implementation of return-policies in Pharmacies is more important than ever with the ongoing pandemic and the resulting increased use of antibiotics, so that left over, unused and expired antibiotics can be dropped off on-spot or mailed to them. And pharmaceutical companies must be held responsible for the appropriate destruction or recycling of these antimicrobial medicines.
We must all understand the scale at which our actions affect the public health, especially those of our loved ones. With resources being at the edge of their limits, and a pandemic straining the healthcare system, it is now more important than ever to become self-aware and promote safe and responsible use of Antimicrobials, besides doing our best to stay well and maintain personal hygiene, keep our environment clean and sanitize our belongings. Prevention is certainly better than cure, and our only hope in reducing the curve. The initiatives we take can save several lives including our own.